Why should you go to a nutritionist?
According to the regulation of healthcare professionals, a Dietitian-nutritionist is the healthcare professional legally qualified to perform diet and food-related activities for patients (always individualising the recommendations according to the physiological and/or pathological conditions), and to provide nutritional advise and treatment.
Currently, we live in the era of information, and it is becoming increasingly easier to find food-related advice and recommendations in magazines, newspapers and, of course, on the internet. However, it is very important to take into account that not all the information available out there is reliable and up to date. What it’s more, all of this flood of information is very ambivalent and what according to a source is beneficial, it appears as the opposite in a different one. This is why you can find arguments to support a position as easy as to disprove it. Hence the importance to attend a dietitian-nutritionist who will provide with individualised recommendations and always with scientific evidence.
What exactly is a dietitian-nutritionist?
It is very often that when people hear the word “Nutritionist” the first thing that comes to their mind is “lose weight” and “dieting”. However, a dietitian- nutritionist is a healthcare professional whose functions go far beyond this, as they are experts in nutrition and dietetics who not only manage the nutritional treatment in a wide variety of conditions and the nutritional approach in all the stages of life, but also the quality management, food security and, lastly, the prevention of lifestyle and nutrition-related conditions.
A Dietitian-Nutritionist will provide individualised recommendations not only considering the general situation of the patient, namely age, stage of life, associated conditions and so on, but also other personal situations, such as their culture.
When should I go to a Nutritionist and how can it be helpful?
These are some of the reasons why you should attend a consultation:
- Change of dietary habits to help prevent lifestyle-related conditions such as type 2 diabetes mellitus, hypercholesterolemia or hypertension, as well as contribute to the nutritional management once diagnosed. In these cases, nutrition is the first line of action, and even when pharmacological treatment is necessary, nutrition is still a key part of the treatment.
- Specific moments in a woman’s life such as pregnancy or breastfeeding. In these stages, the nutritional requirements are increased, and it is essential to ensure an optimal nutrition intake from all macro and micronutrients.

- Nutritional approach in all different stages of life from childhood to advanced ages in both health and disease, and always considering the singularities of every different stage.
- Infant nutrition. Dietary advice in transitioning from exclusive breastfeeding to solid foods, that is, how and when to introduce the different solids gradually. Also, with the baby-led weaning (BLW), which has been on the rise in recent years: precautions, benefits and inconvenients, which foods and how to cook them, textures and much more.
- Optimisation of the sports performance in order to adapt recommendations according to the type of sport discipline and individual requirements as well as to assess potential needs for supplementation to enhance performance.
- Gut disorders: fructose and sorbitol intolerance, Small Intestine Bacterial Overgrowth (SIBO), non-celiac gluten intolerance, celiac disease, Chron disease or ulcerative colitis.
- Nutritional management in other conditions such as renal disease or cancer. Also, in hormonal problems such as hypothalamic amenorrhea.
- Learn how to eat healthily and nutritional education. You do not have to be sick or have a specific situation to attend a Nutritionist. Sometimes a person might just want to learn how to eat better and make a habit change.
- Vegetarian diets. Either due to animal welfare reasons, the environment or because of other personal arguments, sometimes a person decides to reduce or eliminate the animal-derived products from their diet to some extent. In any case (ovolactovegetarian, vegan…), a nutritionist can assist in making the transition progressively, and can also provide alternatives to substitute all these products for other plant-based options to make sure that all the important nutrients are covered.
In summary, our health is very important and for that reason we should always aim to find qualified healthcare professionals to always make sure that the dietetic recommendations will be coherent, evidence-based and individualised depending in the individual circumstances.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
A Superhero therapy tool kit to help your children cope with difficult situations
Superhero therapy, is that a thing?
Janina Scarlet PhD, adapted an evidence-based therapy called Acceptance and commitment therapy (ACT) and turned it into the superhero lover’s dream. To help children and adults manage their symptoms of depression, anxiety, post-traumatic stress disorders and other mental health conditions. ACT and Superhero Therapy’s objective is to help people learn to have a healthier, more flexible relationship with their thoughts, feelings and other significant private events. Which in turn will allow them understand who they want to be and to move towards what is truly valuable to them.
Working on values with children can be a very challenging task given its abstract background. Asking children or teens to do what is important above all pain or discomfort might seem impossible. Fortunately, That is where superheroes come in handy. Using an ACT framework, a therapist can help a patient relate to a fictional superhero, understand that superhero’s origin story and discuss how that superhero has overcome many of their own challenges (probably social, emotional or psychologically related) by taking actions toward their values (Washington, 2019). Prompting children to connect with a superhero’s story will allow them to play with different perspectives which can help them clarify what is important to them.
So how can we use superhero therapy in our everyday life?
Ideally, superhero therapy should be used as a guideline for evidence-based therapists to use with children or adults in session. However like Marvel Comics creator Stan Lee said, “The person who helps others simply because it should or must be done, and because it is the right thing to do, is indeed, without a doubt a real superhero.” So grab your cape and lets bring out our superhero within.
1 – Find a superhero your children can relate to. Can you think of a superhero or a character your child can relate to? It can also be their favorite character, it does not have to be a superhero in a strict sense of the word. It can be any character in their favorite book, movie or series. It can even be a family member or a person in their life they admire. A character that might have an origin story or a struggle they can relate to.
For example, for Dr. Scarlet it was Storm from X-Men. When she was very young, Dr. Scarlet was exposed to a nuclear explosion because she lived in a small town near Chernobyl. This had incredibly debilitating effects on her health. To make matters worse, her symptoms where heavily influenced by the weather, if it was hot outside she would get severe nose bleeds, if it was humid she would get migraines or seizures and so on. When she was twelve her family decided to move to the United States, thinking the situation would get better being away from radiation but there she faced other types of struggles. In school her new classmates could not understand what she had gone through. She had to endure intense bullying, she was called radioactive or contagious, her peers were afraid to touch her or be near her. This made her feel completely alone and depressed but it all changed when she watch X-Men. The “Super mutants” made her feel less lonely specially when she discovered Storm a superhero who could control the weather. A superpower she always wished to have since her own struggles depended on the weather.
Is there any superhero that could make your child feel a little less alone in the world. A character they love or admire? It can be Batman, Ironman, Hulk, Harry Potter, Katniss Everdeen, even a Disney princess, a character from Encanto, Frozen and anime series. Anything you can think of.
2 – What is their superpower? Try to find out what is it that your kid loves so much about this character. What superpowers do they have. What struggles have they faced and what have they needed to overcome them. What are they like, what characteristics have hook you child to this character. This is a conversation you can have with younger children too, they might not be as clear as older children but if they tell you they like batman because he is good at getting out of trouble there are a couple of characteristics you can take away from that, like smart, problem solving, quick, strong. There is always something behind the obvious answer, this superpowers might be the window to your children’s values.
3 – Superhero diary. Once you have found the superpowers your child looks up its important they are translated into actions. Find a way you and your child can be a little bit more like Superman, Batman, Elsa, Katniss or whoever you have chosen. To make it more fun think of them as special missions and write them down in a Superhero Diary where your child can draw or write all the things they have done like their superhero so they can come back in difficult times and remind themselves all they are capable of.
4 – Find a Superhero Mentor. Every Superhero has a sidekick or a mentor who supports them during their missions. Batman has Alfred, Harry Potter has Ron and Hermione, Ironman has Jarvis, Katniss has Haymitch. Encourage your child to find a sidekick or a mentor it can be a family member, a friend, a pet or even a therapist or a counselor. Sinews can be a great source for counseling, we great group of child therapists that will gladly jump at the chance to be a superhero mentor.
5 – Every superhero journey starts with a struggle. Last but not least remind your children that all superheroes have an origin story that usually involve some kind struggle. Batman lost his parents, Harry Potter not only lost his parents he had to endure the horrible family he had left, Hulk was exposed to radiation. This stories turned them into the superheroes they are, the struggles helped them develop the incredible superpowers that we all admire. So if your children feel like life is a little daunting remind them it will turn them into amazing superheroes.
References:
Scarlet, J. (2017). Superhero Therapy: Mindfulness skills to help teens & young adults deal with anxiety, depression and trauma. New Harbinger.
Washington, K. (2019, April 25). What is superhero therapy?. Denver Health Blog. https://www.denverhealth.org/blog/2019/04/what-is-superhero-therapy
Sinews MTI
Psychology, Psychiatry and Speech Therapy
The importance of setting limits and how to do it: children and adolescents
We encounter daily situations of «disobedience» on the part of children. It is normal and necessary that it happens when the child is in the moments of consolidation of his individuality. And even more so when dealing with people with whom the emotional involvement is intense, so we should not feel like victims.
There are always difficulties and contradictions when educating children but let us keep in mind that the lack of consistency and clarity in transmitting the rules makes children insecure and nervous (more crises, tantrums, and whims). Those who live with the child must agree on the rules and educational guidelines that will be asked.
If disobedience is continuous, we should think that the child is not happy and that he/she is asking for help.
Why do they sometimes provoke us?
The child loses limits easily, which distresses him, so he calls the adult to see if the same thing happens to us and to know with our example how to react. What reassures him/her is to see our security (it is not that he is asking for a spanking to calm down).
As adults, we must adapt our authority to the new individual who is growing up, with his own desires and rights that come up against the limitations corresponding to the desires and rights of others.
What are boundaries for?
Throughout their growth, children need limits and rules that help them know their possibilities, how far they can go, and what is expected of them. It is about providing a frame of reference and not so much about what to do when the child becomes «impossible».
Limits help them grow, while punishments create anxiety and low self-esteem. Through them, you can teach your son or daughter self-discipline; he or she will learn to deal with his or her own responsibilities without being reminded, developing strategies to impose limits on himself or herself.
The first limits have to do with the care provided to the baby in the attention to his basic needs, and allow him to differentiate little by little what he is from what others are, the internal and the external, with which he will be able to advance in the organization of his personality.
Limits will also help the child learn to deal with uncomfortable emotions such as frustration, anger, boredom, or sadness. Every boundary is an opportunity to learn to manage emotions.
Through boundaries, we teach our children that we care about them. Very often, children test limits to see how adults will react. Implementing negative consequences for breaking the rules shows that the adult is not letting the situation get out of control, creating security in the child.
Thanks to limits, he/she will learn to be able to postpone the immediate satisfaction of his desires, which favors coexistence and socialization. They will also be able to advance in their autonomy, from the external control provided by the adult to the development of their own criteria, being responsible for their actions and self-control.
How to set boundaries?
When setting boundaries, we must consider certain factors that will help us to do it correctly:
- Be clear that limits are necessary for the child.
- Be calm when we request or prohibit something from the child, so he/she will be more willing to comply with what is asked of him/her. That is to say, do not wait to set limits when they have already exceeded our patience.
- If the child reacts to a small frustration with a tantrum, we must wait until it passes, restrain him physically if there is a risk of injury, and then put into words what has happened («you got angry because of…»).
- When we forbid something, we can offer the allowed alternative. Knowing how to give him alternatives helps them learn to decide.
- It is better to select and establish the highest priority that we are going to ask for and wait until it is achieved, rather than trying to make him respect new rules. Neither wear out our authority in the face of unimportant details nor fall into the extreme of «let them do it» for everything.
- Offer explanations or reasons to justify the demands («it can break… «you can hurt yourself… «it is not yours…») without trying to justify ourselves.
- Do not try to discuss the reason for the limit. It is enough to give a reasoned explanation of the expectation we have, sometimes silence is a powerful tool.
- Few commands, but clear and expressed in a positive way (negative commands invite rejection, create more resistance and desire to transgress them). In other words, express what you want, not what you don’t want.
- Make sure that the rules are appropriate to the child’s maturity level (make sure that the child understands them) and that they are coherent, not contradictory or arbitrary. And also, they must be true.
- The limit must be set in time and the child must be made aware of it, and even know how much time he/she has to react to the proposed rule. We cannot always demand immediate obedience as soon as we try to set a limit since we are not looking for a submission but for learning.
- Involve your son or daughter in the creation of limits or house rules. In this way, not only are they motivated to follow the limits and routines by having participated in their creation, but they are also learning problem-solving skills.
- Let’s try not to mix up the different situations; it’s not the best time to «teach» rules when we spend time having fun through play and conversation.
Setting boundaries in adolescents
In adolescents, being able to set boundaries is one of the best ways to improve communication and build more trust, thus reducing conflict. At this age, knowing how to set and shape boundaries (perhaps from when they were younger) forces you to recognize the fact that your son or daughter is growing up and needs the control established when they were younger to be loosened and adapted to their new circumstances so they can mature.
It is especially important in adolescents that the limit be very clear; the following formula can be used:
Limit or rule (what is not allowed) + exceptions to the rule + consequences of not complying.
Important points to keep in mind when setting limits for adolescents:
- Be consistent with the rules, it is especially important to agree with everyone in the house on what the limits are and not to forget to apply the consequences. Adolescence is a period in which it is normal to try to find inconsistencies in the rules we are given in order to break them.
- Allow them to understand the natural consequences of their actions and decisions. Many times, it is not necessary to set a limit but to make your son or daughter understand that he or she will be responsible for the consequences of his or her actions. For example, if their actions result in a financial cost, they will be responsible for paying for it with their own money, or they will do a chore around the house that is monetarily equivalent.
- Respect in the same way you want to be respected. Adolescents are beginning to create their own identities and understand their place in the world, and to do so they need to feel respected as individuals by their parents. It is through mutual respect that we manage to set limits that they themselves choose to respect.
At the end of the day, we have to remember that rules and limits are essential, but from the support, affection, and above all the understanding that makes us understand the struggle between complying with certain rules and limits and the child’s need to assert their independence and autonomy.
We must find a balance between the socialization of our children and their need for affirmation, autonomy, and independence. It is from here that they will be able to face the negative emotions that appear throughout their lives without having to recur to alternative ways (alcohol, drugs, violence…) to manage them.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
Is dyslexia affected by bilingualism?
Question:
My child is bilingual, and we have just detected that he presents dyslexia, should we remove one language?
Answer:
Dyslexia is a specific learning disorder of neurobiological origin. It is not related to low intellectual abilities, poor schooling, laziness, or the number of languages that your child speaks. Dyslexia is not related to oral language, so your child will be able to speak as many languages as he/she wishes.
Within dyslexia, we can differentiate between decoding difficulties and comprehension difficulties. The first ones stem from phonological deficits and it is related to being able to associate sounds and letters. In contrast, comprehension difficulties are associated with vocabulary, morphological and pragmatic skills.
We can find two types of orthographies when writing and reading a language: transparent orthography, the grapheme-phoneme correspondence is clear (like Spanish) or opaque orthographies, the correspondence between grapheme-phoneme is not as straightforward (like English). Some authors suggest that learning to read in both, opaque and transparent languages, would help people with dyslexia compensate for their deficits in phonological decoding by transferring phonological awareness and sublexical decoding abilities from consistent to inconsistent orthography.
I would like to stress the need to receive therapy in both languages because the needs will be specific to each language.
All in all, bilingualism doesn’t cause dyslexia nor does it increase the risk of presenting it, so there wouldn’t be a need to stop using one language. Some authors even say that bilingualism may have some benefits for dyslexia. The only thing is that your child will need to have therapy sessions in both languages because each language is different, and he/she will have different needs in each one.
Although it will take some effort, it will be possible for your child to achieve a good reading and writing level with the right approach. If they find it very difficult to keep up with one of the languages and you chose to remove one of them, I would remove the one they use the least in reading and writing form. But that doesn’t have to be a choice as they will be able to read and write in both of them.
If you need more help regarding this topic you can click here to get your online appointment with us.
References:
- Do Amaral J. & de Azevedo, B. (2021). What research can tell us about the interaction between dyslexia and bilingualism: an integrative review. Letronica, 14(2), 1-17. https://revistaseletronicas.pucrs.br/index.php/letronica/article/view/38695
Sinews MTI
Psychology, Psychiatry and Speech Therapy
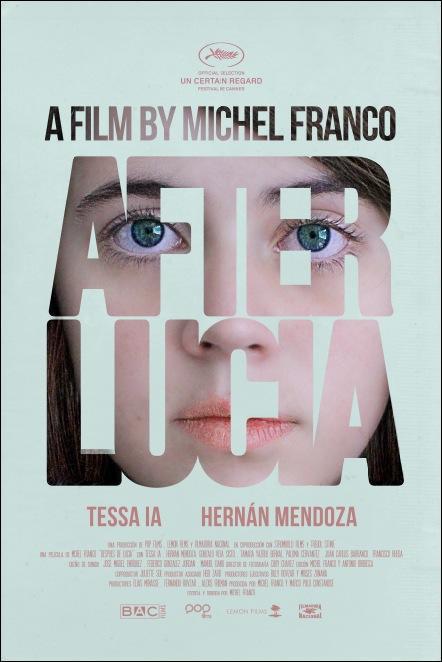
After Lucia: Grief, Bullying, and Violence
After Lucía is a Mexican production that deals with issues such as bullying and violence in the classroom in a raw and cold way, intertwining this main theme with problems such as grief, lack of limits in adolescents, and lack of emotional management skills among many others.
The film tells the story of Alejandra, who moves to Mexico City with her father after the death of her mother in a traffic accident in which she was present. There, a series of events is unleashed that give rise to bullying that escalates until it explodes. The tragic death of Lucia, the mother, has turned Roberto (the father) and Alejandra into vulnerable beings, who have not yet overcome their grief. Hence the title of the film, since this vulnerability is a facilitator for the bullying to occur to such a high degree, the protagonist not being able to count on her father as a source of help and support.
The film takes care of disconcerting the viewer, using a very slow and realistic narrative, in which we slowly get to know Alejandra, and together discover all the hardships she is going through. At times one might think that such coldness in the face of suffering is impossible in young people, but reality can surpass fiction.
Unprocessed grief
In the first half of the film, we see several scenes in which the director subtly reflects the lack of a healthy processing of Lucia’s grief. The first scene shows how Roberto picks up the car from the accident at the mechanic’s shop and leaves it abandoned on the street, with no explanation to the viewer as to what is going on. We also see how Alejandra says that her mother stayed in Porto when asked about her, or how Roberto does not want to use the same things from the old house. Through these examples of avoidance in the face of the impossibility of facing reality, in addition to small details and many walls of silence and sudden explosions of emotion, Michel Franco lays the foundation on which all the subsequent violence is maintained.
The Bullying
Alejandra’s relationship with her classmates begins as normal, a new girl who joins the popular group, they go to a party, drink and do drugs together and she has sex with one of them, who records everything. Here we begin to see Alejandra’s self-injurious behaviors, who agrees to be recorded without imagining what could happen next. The virtualization of the video at school is the trigger of harassment that increases exponentially, going from verbal annoyances to physical and sexual violence and social exclusion, being ignored, while she suffers all kinds of mistreatment. In addition, it is seen how electronic devices facilitate the rapid increase in harassment.
To understand the film, it is necessary to look at the phenomenon of naturalization of violence in schools, which is becoming more and more established, becoming a «normal», «everyday» violence.
Causes and consequences of bullying in After Lucia
We see how Alejandra’s relationship with her father is apparently good and «relaxed», which is in reality quite fragile and superficial, with no trust and based on lies and cover-ups, making the protagonist more vulnerable. She has no support to defend herself, recently orphaned from her mother, with a father who doesn’t know how to devote quality time to her, being the new girl who needs friends no matter what. There is also latent guilt in Alejandra for the death of her mother, which is never explained to the viewer; this guilt may be the cause of the passive attitude she shows in the face of harassment, almost implying that «I deserve it».
Where are the adults?
Something that is very evident throughout the film is the lack of adult presence, not only on the part of Roberto who does not find out until the end of what is happening to his daughter but also from teachers and parents of other students. There is a scene, in which we see how they mistreat Alejandra on her birthday after a class in which we do not see a single adult intervene in any way, although this happens inside a classroom of the institute. Neither in meetings at classmates’ homes nor on school trips, do we hardly see the presence of adults setting any kind of limits.
The social tribe
One of the greatest complexities in adolescence is the codes generated among peers. One of them, latent in this film, is that denouncing is equivalent to exclusion since the one who takes it «puts up with it». Alejandra abides by these codes fiercely, being the moment in which she lies when asked directly what is happening at the point of no return. Here the aggressors are aware of their impunity and everything begins to unfold at breathtaking speed.
We also observe the establishment of roles and the desperation to get out of the role of the victim. We see at the beginning that one of the boys in the group is the one who fulfilled this role before Alejandra arrived, being an overweight adolescent. As soon as the ban is opened to harass the protagonist, this is one of the characters who harasses more strongly, since he sees the opportunity for someone else to take the role he had been playing until now, and feels that he belongs to the group in a stronger way.
The consequences of bullying that we see in Alejandra are evident: anguish, sadness, isolation, social phobia, learned helplessness, anxiety, suicidal ideation, and depression. The aftermath of bullying usually accompanies people into adulthood, resulting in depressive adults, with a tendency to addiction or prone to develop a psychological disorder.
Conclusion
After Lucía is not an «easy» film but a hurtful, uncomfortable, and raw film that makes you feel the hopelessness of the protagonist and generates feelings of anguish, helplessness, and rejection. The great achievement of this film is that it makes you feel the pain of the characters. The viewer finds himself wanting it to end or for something to happen that generates some kind of justice… and the ending will not leave any viewer indifferent.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
Is my child’s language development normal?
Language is the main form of communication between people. This article will focus on spoken language.
The first three years of life are fundamental for its development as the brain is in the process of maturing and is when it is in an optimal state for the acquisition of these skills.
Among language disorders, we can differentiate between receptive (comprehension difficulties), expressive (production difficulties), and processing disorders.
Regular development of oral language in a kid:
Between zero and four months, babies are usually calmed by their mother’s voice and show a clear interest in other people’s faces. On the other hand, they can express different things through crying, such as for food or comfort. Crying is one of the first acts of communication because through it they learn that they can alter their environment. In addition to crying, they begin to smile socially and laugh.
At six months, they can respond to their name, follow auditory stimuli with their eyes and begin to babble and vocalize. This is followed by the understanding of verbal routines, such as «bye-bye» and pointing and saying first words, which usually happens around nine months. At around twelve months, infants can follow a verbal command and produce three meaningful words (e.g. «mommy», «daddy», «water»).
At fifteen months, children can identify their body parts when asked about them (asked «where are your legs?» the child will be able to point at them). In terms of expression, they acquire more vocabulary.
Between eighteen and twenty-four months, they will be able to recognize their body parts, as well as to follow simple verbal commands. Production is characterized by an increase in the number of words they use, they have a vocabulary of around 50 words and can make two-word combinations («more bread»). In addition, they know their name and can use it.
From twenty-four to thirty-six months, children understand and carry out complex verbal commands and can make three-word sentences. In addition to this, they can use the interrogative particle «what» to formulate questions. They also begin to use pronouns such as «you» or «I», understand «you», «me» or «she», and respond to simple questions.
Between 36-48 months, understanding of actions and the use of the question «why?». Between 48-60 months, children can understand everything that is said to them, as well as generate complete sentences and tell stories. At this stage, they understand spatial terms such as «behind» or «beside». Errors in long and complex words such as «hippopotamus» are considered typical, but a person outside the child’s immediate family can understand and carry on a conversation with the child.
Finally, by the age of six, they can understand and carry out commands of all complexity and have the ability to express themselves without making errors related to the articulation of sounds as well as narrate events and make-up stories.
The typical development of a child’s language in the different stages of childhood has been described above.
Red flags:
There are a series of red flags that will allow us to identify whether the child’s language is as expected for his or her age or if, on the other hand, a specialist should be consulted.
Between the first and fourth months, the presence of a bizarre cry and the absence of a social smile should draw attention.
On the other hand, between the sixth and ninth months, one should pay attention to the lack of vocalizations and babbling, as well as frequent bisyllabic words such as «mummy/daddy».
At twelve months, the loss of already acquired skills is a warning sign.
On the other hand, at fifteen months the child should be able to point and use three-word combinations, if not, a specialist should be consulted. Another warning sign is the failure to follow simple instructions, recognize body parts, and say at least 25 words between eighteen and twenty-four months. After that, at thirty-six months, they should be using two-word sentences and following two-command instructions.
From thirty-six to forty-eight months, the use of incorrect words or the replacement of one word with another should be brought to our attention. Finally, from forty-eight months to six years, inappropriate use of speech, i.e. the presence of speech with errors in the production of sounds, as well as the inability to tell a story or follow a conversation, is considered alarming.
In conclusion, although each child’s development is unique, a certain age must correspond to the achievement of defined milestones. If this is not the case, it would be advisable to consult a speech therapist who will be able to resolve any doubts or concerns.
|
AGE |
RECEPTIVE LANGUAGE |
EXPRESSIVE LANGUAGE |
RED FLAGS |
|
0-4m |
Are calmed by the mother’s voice. |
Crying, social smile, and laugh. |
Bizarre cry. Absence of social smile. |
|
6m |
Respond to their name. Follow auditory stimuli with their eyes. |
Babbles. |
Lack of vocalizations and babbling. |
|
9m |
Verbal routines like “bye-bye”. |
First words. |
Lack of bisyllabic words like “mummy/daddy”. |
|
12m |
Follow verbal commands. |
Produce three meaningful words. |
Loss of already acquired skills. |
|
15m |
Identification of body parts. |
More vocabulary. |
Not pointing and using the three-word combination. |
|
18-24m |
Recognize body parts, follow simple verbal commands, and recognize their name |
Increase in the number of words (around 50). Use their name and make two-word combinations |
Failure to follow simple instructions, recognize body parts, and have a vocabulary of 25 words. |
|
24-36m |
Understand complex verbal commands. Understand pronouns (“you”, “me”, or “she”). |
Make three-word sentences. Questions with “what”. Use pronouns (“you” or “I”). Respond to simple questions. |
Failure to use two-word sentences and following two-command instructions. |
|
36-48m |
Comprehension of actions. |
Questions with “why”. |
Use of incorrect words. |
|
48-60m |
They understand everything. |
Produce complete sentences and tell stories. |
Presence of sound errors. Inability to tell a story or follow a conversation. |
- Moreno-Flagge, N. (2013). Trastornos del lenguaje. Diagnóstico y tratamiento. Revista neurológica, 57 (supl 1), 85-94. https://d1wqtxts1xzle7.cloudfront.net/60986065/1.-_Trastornos_del_lenguaje_diagnostico_y_tratamiento20191022-80419-h1p56m-with-cover-page-v2.pdf?Expires=1652004561&Signature=BTaA56uiJzgG40OY7QV6LEfFWwdhz7j1r83-xNISv~ZFQgVB~e9ZM9Guur7juc0X2JunzZcKZ-RvSZTIg2L7Z2y6BhM-tFsQIDVkNMWAqwx~VpKzh3IugK-ER9wf1T6PU-vGZIUFWLtXwIKhhJG1R~SyMCoikRHyhfU6sbdqFDldnyP2CyUqt4QGDlJI-EW-Yk7vqSHMJ8UCpXR2F~pZrp-YHG5cjtXSRauUkp4M8nebltf0JmzcmYQMGfdRCYNKj4tHJ2H28vNHrcu1K2VApze7z7t8up0B3YMko9O4YCSQbXCsTQ2qUYJmoMVhmMvPA9dPTmuVyyk3YzN~PzgmHA__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA
- National Institute on Deafness and Other Communication Disorders. (2017). Speech and Language Developmental Milestones. https://www.nidcd.nih.gov/health/speech-and-language
- Galeote Moreno, M. (2007). Adquisición del lenguaje. Problemas investigación y perspectivas. Ediciones Pirámides.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
Attached, a book to better understand your love relationships
Love is, without a doubt, one of the subjects that have fascinated us most (and tortured us, in equal parts) since the beginning of civilization, but also one of the great scientific questions: how does love work and, above all, why do we fall in love with whom we fall in love? In psychology, one of the theories seeking explanations, investigating, and solving, in part, these enigmas is the attachment theory.
The beauty of this theory is that if we know our attachment style, we can also resolve some of the love contradictions we fall into and make better romantic decisions. For example, «Why is it that if, in general, I consider myself a confident person, the moment the guy I like behaves distantly with me, I feel terrible and like I’m worthless?». Perhaps someone else is wondering: «I normally have no problem falling in love, but why is it that when the relationship becomes steady, I start to find they have too many flaws and decide to break up quickly?»
First, let’s put this theory in context: Initially, the study of attachment was not related to romantic relationships but to the bond that arises between infants and their parents or affectionate caregivers. In 1958, Bowlby, an English psychiatrist working in a hospital with children, coined this term when studying the effects of the mother-child relationship on the infant’s cognitive, emotional, and social development. Even if their physical and nutritional needs were met, the babies who had been prematurely separated from their mothers (because, for example, they were orphans during the Second World War) suffered serious consequences in their cognitive development due to the absence of contact with their attachment figure.
Thanks to this theory, we learned that when we are born, we need the protection of an adult to meet our physical needs – such as food and shelter – but, above all, we need the bond to feel loved, cared for, and comforted when our nervous system and stress response are activated.
It was not until much later, in the late 1980s, that Cindy Hazan and Philip Shaver helped us understand that the need for attachment is not unique to children. The security we feel or don’t feel in our romantic relationship also awakens our attachment styles. To put it simply, the bond created in our relationship with our parents functions as the blueprint for understanding our expectations in our future intimate and social relationships.
In this book, ‘Attached’ by Levine and Heller (2010), they take an in-depth look at how our attachment style influences the romantic decisions we make.
As children, people with a secure attachment style learned that the world was a stable, predictable place. They felt they could trust the people around them to be available whenever they needed them. That is why they tend not to feel much doubt in their romantic relationships. They feel comfortable showing themselves vulnerable to the person they love. In general, they feel deserving of such affection.
In contrast, people with an anxious attachment style grew up in an environment in which their physical and emotional needs were met ambivalently or intermittently: at times, they were there to care for them, and their affectionate caregivers understood what they needed, and at other times, they were not there or did not feel available to them. As we know, infants’ primary goal is to ensure their proximity to their attachment figure. That’s why children with an insecure-anxious attachment developed a very adaptive strategy to achieve this: to get even closer to their attachment figure especially when their caregiver moved away. As an adult, if you identify with this style, you probably criticize yourself a lot. When the person you like is distant or ambivalent, their attitude generates a lot of anxiety within you. To calm yourself down, you seek to get even closer to them. Please do not criticize yourself or call yourself «desperate» remember, in the past; this was an adaptive way to survive.
People with an avoidant attachment style learned that their caregivers might reject them or be distant from them. Therefore, they learned to rely only on themselves and not count on anyone else because if they were too trusting, they were afraid of being hurt later on. In their romantic relationships, they say they want intimacy and closeness, fall in love easily, and have no difficulty having intimate sexual relations. However, as soon as they deepen a relationship, they are afraid of losing their independence and become distant.
This book helps us identify our attachment styles and, from that knowledge, to take steps to find relationships that «heal» us. Specifically, it explores in depth the affective needs that each style possesses. For example, people with an anxious attachment style will need frequent contact, stability, clarity about what the other person feels, etc. Having these needs is valid, and more than that, it is essential to be aware of them and seek romantic relationships that are aligned with those needs. If we validate our own needs and communicate them openly, we will observe how our partner reacts and if they are ready to meet our needs (or not). From there, it will be easier to decide to prioritize relationships with people who offer us a secure base and transmit the affection and trust we need so much.
In ‘Attached’, we can have a first approach to attachment theory and how it influences our romantic relationships. But, in this book, several issues are left out; for example, the book does not reflect examples of LGTBQ+ relationships. Nor does it attempt to explain how attachment styles would influence polyamorous or non-monogamous relationships.
In any case, I think this book is an excellent start to reflect on your romantic choices and catch yourself on toxic patterns before they happen.
Good luck on this journey finding healthier relationships!
Division of Psychology, Psychotherapy and Coaching
Psychologist
Adults and adolescents
Languages: English and Spanish
“Nine perfect stangers” and the danger of pseudo therapies
The premise of this Amazon Prime series is simple: nine people go to «Tranquilum», a peaceful and luxurious resort in California, which promises healing and a change in their lives in a few days. But almost nothing is as it seems. As a mental health and psychological wellness professional, there are many reasons why I recommend this series.
First of all, because of the characters which are all very well designed: they are all people with very different backgrounds and different life stories. Among them I would highlight a family that has not yet overcome the terrible grief following the suicide of their eldest son three years earlier, a best-selling writer in the dumps both professionally and personally, a depressed former elite athlete, bitter and addicted to painkillers, an insecure and angry recently divorced woman, a young couple newly rich thanks to winning the lottery living a very shallow life. Also the character who is the director of the center, Masha (played by Nicole Kidman), shows us a very complex person, who faces serious traumas from her own past. In general, through the experiences of the characters who come to Tranquilum in search of healing and improvement, we see very serious problems such as mourning for the loss of a child, suicide, loneliness, post-traumatic stress disorder and depression.
I also recommend it for the moment we are living in.
The growing need for mental health services is a clear trend in Spain and in the rest of the world and that undoubtedly has been increased by the effects of the pandemic. For this reason, I believe that “Nine Perfect Strangers” is a series that, aside from its undeniable cinematographic qualities (it has a first-class cast, a fast-paced script, and manages to move in a rather crazy but always successful way between comedy, drama and a thriller) is seen with different eyes today, since it hits close to home for many people. After all, the pandemic has made visible the large number of people who suffer and need psychological or psychiatric care. Also why isolation, loneliness and suffering have increased and in the series, despite the wrong environment, the protagonists initially experience something similar to support thanks to the fact that they are sharing their experiences and traumas with other human beings who have suffered and need help. The impact of sharing our experiences with other people is well recognised as a healing process in group therapy, although the way this is done in «Tranquilum» makes any healing and improvement impossible.
Among the few unorthodox therapeutic methods used in Tranquilum is the use of hallucinogenic drugs. Without a doubt, it is a much more niche trend in the real world, but it is not non-existent or new for this reason. Although there is debate in the academic world about the scientific evidence that in very controlled contexts and in very small doses, the consumption of certain substances, under the supervision and guidance of a qualified mental health professional, can help in the therapeutic process, the series shows us the dangers of the uncontrolled use of hallucinogenic substances with supposed curative purposes when it is done in excessive doses, without supervision or with the supervision of the wrong person, who is not qualified. In general, in everything related to the use of hallucinogenic substances, prudence is what is called for.
Finally, in the series we also see reflected an increasingly widespread trend in many areas of life but especially dangerous in mental health: the search for quick, almost miraculous solutions to our problems. The lack of time in modern life encourages solutions of this type and it is precisely where professional intrusiveness and pseudoscience sneak in, profiting on the suffering of people, promising the impossible, even without having the qualifications or the knowledge suitable as a professional.
In the end, the characters (actually victims) instead of going to a psychologist or psychiatrist and facing a slow but effective path, prefer to believe the promises of a guru with hidden pretensions who tells them that she will heal them in just a few days. They accept being drugged in an uncontrolled way to face their pain, fears and obsessions. For all this, in addition to being an excellent audiovisual product, intelligent entertainment, «Nine Perfect Strangers» is a series that highlights, in contrast to the dangers of pseudoscience and «alternative» treatments, the importance of the work that mental health and emotional well-being professionals perform, more necessary than ever in the face of the great demand for mental health that the population requests.
Sinews MTI
Psychology, Psychiatry and Speech Therapy
Movie Review: The Break-up (2006)
“The Break-Up” is an ideal movie to understand the inner workings of relationships. It is about Brooke (Jennifer Aniston) and Gary (Vince Vaughn), a couple who decide to put an end to their relationship after some years together, which then leads to a series of circumstances: the fight for who keeps the apartment they shared, and later, the way they both go through this breakup.
A scene that is key happens at the beginning of the movie, where the couple has an argument over superficial matters. Brooke accuses Gary of not helping her wash the dishes, and then continues saying that he never buys her flowers or takes her to the ballet. Gary then responds in a frustrated manner, saying he feels like nothing is ever good enough for Brooke and that she will never be happy with it.
This kind of argument can often happen within relationships, and there are times where the couple may not realize the message that is behind the superficial talk.
Within this couple’s dynamic we can observe how one’s thoughts and actions can feed into the other person’s, and viceversa, therefore creating a vicious cycle (or how we call it in therapy: circularity). In this case, if we reduce this dynamic to a simple mechanism, we would see it this way:
Brooke thinks “Gary doesn’t appreciate me”, therefore she feels like she isn’t valued, frustrated and demotivated. Consequently, she tells Gary that he doesn’t do anything for her. This leads to point number 2.
Gary thinks “Whatever I do, Brooke will never see it as enough”, therefore he feels incapable, frustrated and defensive. Consequently he doesn’t try to do things that Brooke would like. And this leads to point number 1.
Within this circularity, it would be necessary to make changes in order to create a new and healthier dynamic.
Moreover, later we see how Brooke does just this, by communicating exactly what she was meaning to get across in the first argument: she doesn’t feel valued or appreciated by Gary. In fact, we can see how Gary is much more receptive to this kind of vulnerable and direct communication, and therefore doesn’t act defensive because he doesn’t feel like it is an attack.
All in all, this romantic comedy is a tool that can show us how a relationship can become complicated due to dynamics that they can get stuck in and can tend to become chronic. But it can also show us how a small change in the dynamic can open new doors towards change and evolving within the relationship.
You can see the clip of the fighting scene here:
The Break-up Movie (2006)
Division of Psychology, Psychotherapy and Coaching
General Health Psychologist
Adults, adolescents, couples and families
Languages: English and Spanish
Dear Santa...
- LINCE (Lynx): We start with an ideal game to stimulate the selective attention of the little ones of the house. It consists of a round board with images and cards on which only one image appears. The game consists of removing a card and finding the image that appears on it as quickly as possible. The first one to find it wins the round. Ideal for an afternoon with the family! (4-7 years old).
- CUBEEZ: Imagine a hybrid between Mr. Potato and a Rubik’s cube and you will get a glimpse of how Cubeez works. Each player has three cubes with different eyes and mouths. The player who can create the face on the card first wins the game. In addition to having a fun time, we will get to work a variety of cognitive functions such as visual selective attention, spatial orientation and fine motor skills.
(From 6 years old).
- JUNGLE SPEED KIDS: The children’s version of this classic board game is perfect to stimulate the reflexes and visual memory of the little ones. The objective of the game is to remember the position of the animal cards in order to form as many pairs as possible and save them from the lion’s claws. The winner is the player who has managed to turn over the most pairs. Another interesting aspect of this game is that it will allow us to work on behavioral inhibition, since when a player picks up two cards and they do not have the same animal, he/she cannot participate in the game until it is his/her turn again. (From 5 years old).
- CONCEPT KIDS: This game is, without a doubt, one of the most recommended for working on concept formation and abstract reasoning. The objective is to get the rest of the players to guess an animal by pointing out the icons that appear on the board. One of its main advantages is that it does not require the use of verbal language or the learning of reading. Therefore, it is ideal for children from 4 years old.
- ANIMAL ON ANIMAL: A version of the classic Jenga adapted for children, which will test their concentration and visuospatial skills. It is one of those basics that never goes out of fashion, getting the whole family. (From 4 years old).